Our bodies are composed of numerous cells, which are nonuniform. Many cell types exist, each of which plays a specific role depending on the tissues and organs that comprise these cells.
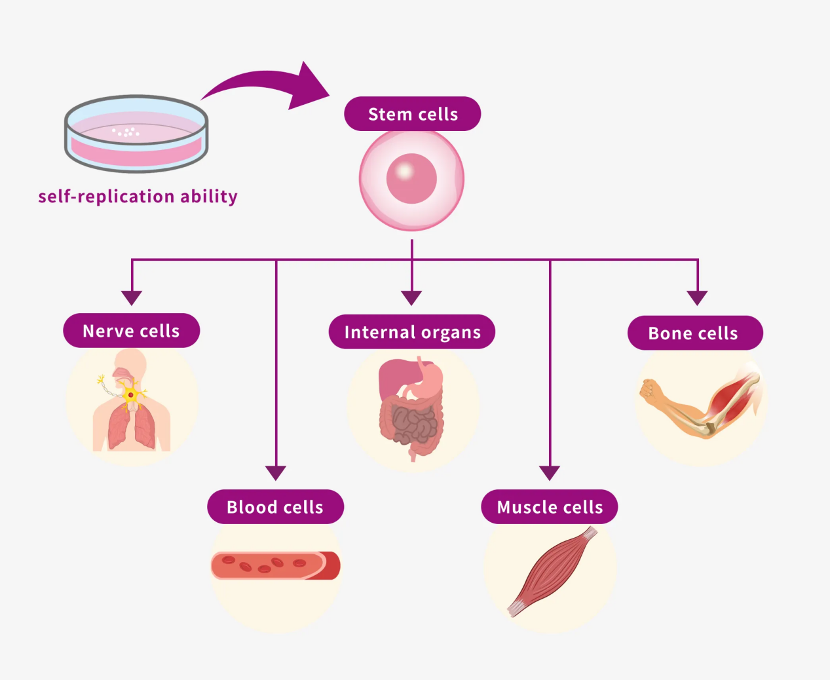
The human body originates from a single fertilized egg that is initially small and undeveloped. As we grow and mature, fertilized eggs develop into a multitude of cells. The growth and development occur because stem cells (which are the precursor cells found in the fertilized egg) divide and differentiate (*Note 1) to generate diverse types of cells that form tissues and organs.
Stem cells in a fertilized egg are called "embryonic stem cells (ES cells)" and have "totipotency," which means that the cells can differentiate into all types of cells. Stem cells that are artificially created using techniques such as gene introduction are called "iPS cells" and have properties similar to those of ES cells.
Differentiation is the process by which a stem cell matures and transforms into a cell with a specific function. Unlike stem cells, differentiated cells have a limited ability to divide and cannot revert into other cell types.
However, the lifespans of these cells were not constant. Cells comprising mature tissues and organs die and are lost owing to aging, disease, or injury. As the old cells die, new cells must be produced to maintain the overall function of the body. This is where stem cells come into play.
Stem cells are present in specific regions of the human body. These cells divide and differentiate to replenish lost cells and help maintain tissue integrity. For example, in the skin, stem cells are found at the base of the epidermis and within hair follicles, whereas in the intestine, they are located in the crypts of the intestinal mucosa.
Blood cells, such as red and white blood cells, are produced from hematopoietic stem cells residing in the bone marrow. Stem cells present in various locations within adult tissues are referred to as "tissue stem cells" and can only differentiate into specific cell types.
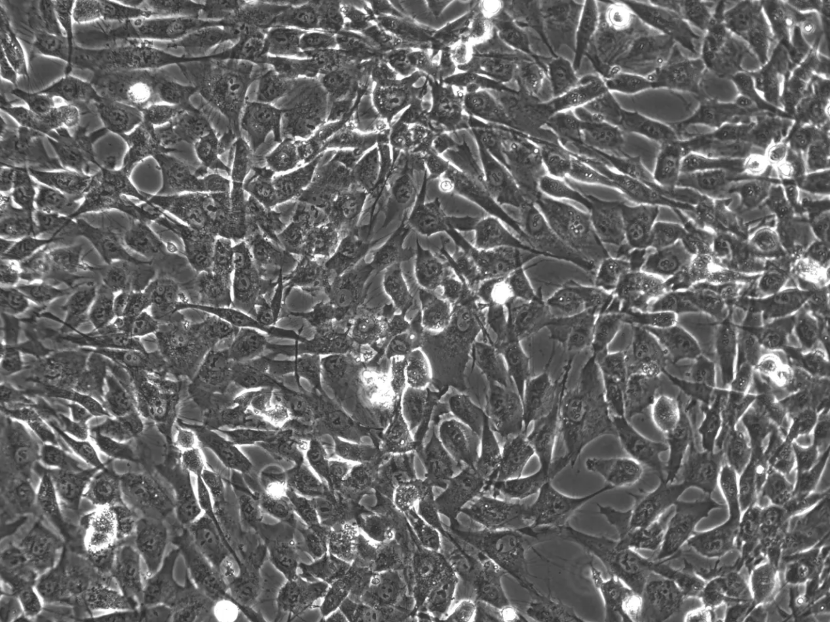
Through research on various "tissue stem cells," scientists have discovered that our bodies contain stem cells with a high potential for differentiation, similar to the ES cells found in fertilized eggs. These stem cells were first identified in the bone marrow in the 1960s and later observed in adipose (fat) tissue in the early 2000s. They are commonly known as "mesenchymal stem cells."

Although ES and iPS cells can form all tissues and organs from a single cell, stem cells lack extensive proliferative and differentiation capacities. However, ES cells can only be obtained from a part of a fertilized egg (specifically, the inner cell mass), which requires sacrificing the fertilized egg. Although surplus fertilized eggs from in vitro fertilization are often used for this purpose, this process poses significant ethical concerns.
In contrast, iPS cells can be generated from adult cells, avoiding the need for fertilized eggs. However, this process involves genetic modifications through gene introduction, which carries the risk of tumor formation after transplantation. Therefore, the safety of iPS cells must be carefully considered. In contrast, mesenchymal stem cells can be harvested from the bone marrow or adipose tissue and have fewer ethical and safety concerns. This makes stem cells a more accessible option for research and clinical applications. Recently, significant progress has been made in the research and clinical application of stem cells, indicating their potential application in regenerative medicine.
Regenerative medicine focuses on artificial creation of lost tissues and organs. This field includes therapies aimed at restoring the function of impaired tissues or organs in a broader sense of the term. Among various approaches used in regenerative medicine, stem cells are the most promising. Stem cells can differentiate into specific tissues and secrete substances known as growth factors and cytokines, which promote the regeneration of surrounding tissues and the formation of new blood vessels necessary for regeneration.
Two main approaches exist in regenerative medicine using stem cells: one involves directly transplanting stem cells to the required site and the other involves differentiating cells in vitro to form the desired organ before transplantation. An example of the former is ongoing research on regenerative therapy that promotes angiogenesis by injecting stem cells into calf muscles to treat peripheral arterial disease, where blood flow to the legs deteriorates. An example of the latter (currently used) is regenerative therapy for severe burns, in which stem cells that differentiate into epidermal cells are cultured in sheet form and applied to the skin.
In Japan, a legal framework for regenerative medicine was established in 2014 (*Note 2), which led to more active implementation of regenerative medicine. Currently, regenerative medicine using stem cells is used to treat a wide range of conditions including peripheral artery disease, burns, cerebral infarction, spinal cord injury, myocardial infarction, liver cirrhosis, and osteoarthritis.
Regenerative medicine aims to artificially create lost tissues and organs. Additionally, it includes, in a broader sense, treatments that restore the function of damaged tissues or organs. Among various regenerative medicine approaches, the use of stem cells is considered the most promising. Stem cells can differentiate into the necessary tissues, secrete growth factors and cytokines to promote surrounding regeneration, and attract new blood vessels that are essential for regeneration.

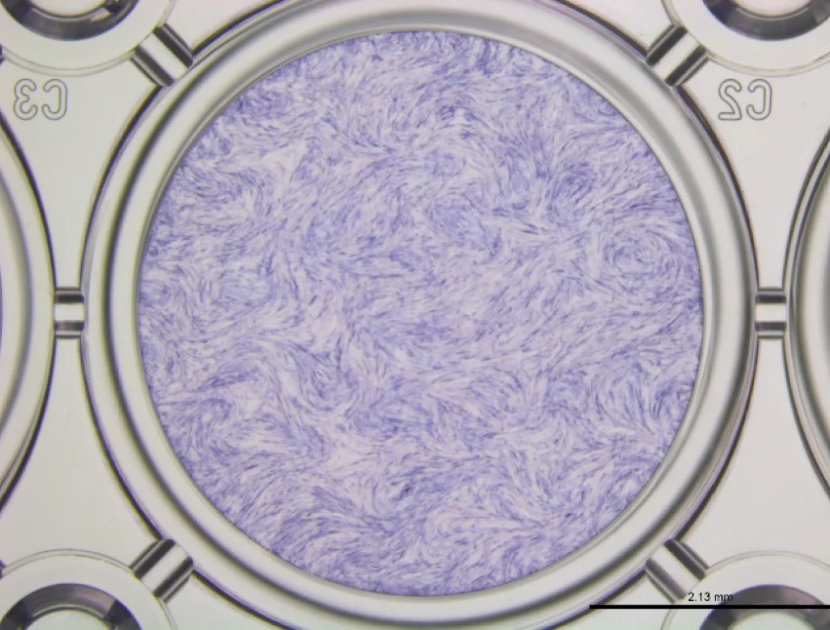
Various types of stem cells are used in regenerative medicine. As mentioned earlier, mesenchymal stem cells can be harvested from bone marrow and subcutaneous fat. Considering that these cells have fewer safety and ethical concerns than ESCs and iPSCs, they can be more easily applied in clinical settings than ES and iPS cells. As of 2024, more than 1,000 plans for regenerative medicine using stem cells other than ES and iPS cells have been submitted to the Minister of Health, Labour, and Welfare under the legal framework. Over 900 studies have used mesenchymal stem cells (*Note 3).
Furthermore, in the "treatment" category of the regenerative medicine provision plans, more than 20,000 patients were treated using stem cells other than ES cells and iPS cells (including mesenchymal stem cells) in the fiscal year 2023 (*Note 4).
In regenerative therapies, it is common practice to extract a small amount of the patient's own tissue, culture mesenchymal stem cells in that tissue, and administer the acquired stem cells to the required area. Mesenchymal stem cells administered to the body can regenerate tissues, improve blood flow, suppress inflammation, and modulate immune responses.

In conditions like osteoarthritis and age-related skin changes (spots and wrinkles), mesenchymal stem cells are injected locally. Conditions such as stroke, liver disorders, and atopic dermatitis are treated systemically via intravenous infusion. These treatment methods are relatively new compared with existing pharmaceutical and surgical therapies. However, their safety and efficacy have only been gradually confirmed. Therefore, regenerative medicine using mesenchymal stem cells is expected to become a common form of treatment in the future.

Natural killer cells (NK cells), a type of lymphocyte that is a part of the innate immune system, has the ability to recognize and attack foreign substances, including cancer cells, without receiving specific instructions from other cells. This is why they are called a natural killer.
NK cells constantly monitor and patrol the body for cancer cells and foreign substances, and its activity tends to decrease after peaking at around age 20. In addition to aging, factors that decrease NK cell activity include stress, lack of sleep, poor diet, and medications. It has also been shown that cancer cells themselves can interfere with NK cell activity. Cancer cells release cytokines (substances involved in transmitting information) in order to escape attacks from NK cells and to try to suppress their actions.
When the activity of NK cells is held back and their function is decreased, the number of cancer cells that cannot be suppressed and kept in check increases.
A technology has been developed in which NK cells are cultured in large quantities outside of the body, activated and then returned to the body. This is our activated NK cell therapy.
This treatment enhances the innate immune system and fights cancer with the power of activated NK cells.
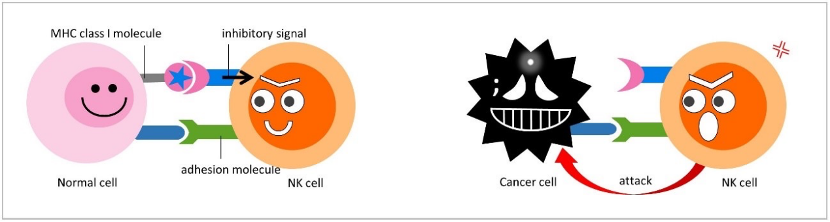
Typically, NK cells recognize cancer cells by using the MHC class I receptors located on the surface of cells in order to determine whether the cell being targeted is normal or not.
While normal cells express MHC class I receptors, cells that do not contain MHC class I receptors are judged to be foreign and NK cells will immediately start attacking.
Many cancer cells do not express these receptors and will be attacked, however, as some cancer cells do express MHC class I molecules, unfortunately NK cells alone cannot attack all cancer cells. When possible, a combined approach of NK cells with the multivalent DC vaccine is recommended as this is more likely to prevent tumor escape.
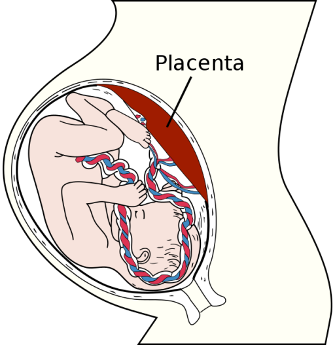
Placenta stem cells are a type of stem cell that is derived from a newborn's placental blood or tissue.
Perinatal is a term that defines the short period right before to right after birth. Women can calculate the approximate gestational age of their fetus and estimate their due date by measuring forward from the date of their last menstrual cycle. To know when your last period started, a period tracker is a useful tool to have.
When the baby is born, blood remains in the placenta. Both the placental blood and tissue are rich sources of perinatal stem cells.
Placenta stem cells include a variety of perinatal cell types, including: